5 Common Skin Conditions/Rashes in Babies/Children
Contributed by: Dr Dave Ong

Our skin acts as a protective barrier, preventing excessive body fluid and mineral loss, helps regulate body heat and protects us against infections
Babies and children generally have sensitive skin which can react to many triggers such as dryness, germs and irritants.
Here are 5 common skin conditions in babies/children:
1. Eczema (Atopic Dermatitis)
The most common skin condition affecting babies and children, eczema usually begins in infancy (3 months and above) or during childhood. 80-90% of cases begin before 6 years of age, 60-70% in infancy and 10% of cases continuing into adulthood.. Eczema is a very itchy condition and is usually chronic and relapsing. It can potentially improve with age and it may even clear completely. However, eczema can still flare up even after an inactive period.
Does My Child Have Eczema?

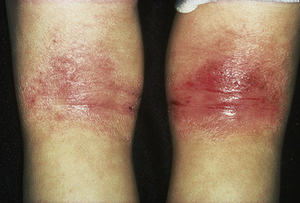

Acute (left) and chronic (right) atopic eczema in the flexural areas of an older child
Atopic eczema appears as red, scaly, scratched rashes. Blisters may be seen. In long-standing chronic cases, the skin can become quite thick. It may present slightly differently depending on the child’s age:
- Infants and babies: Commonly affects the scalp and face, especially on the cheeks. Your baby may be fretful and rub his face frequently. In more severe cases, it can also affect the limbs and trunk.
- Toddlers and adolescents: Commonly affects the areas with folds (e.g. neck, elbows, wrists, ankles and behind the knees). It can become more generalised in more serious cases.
To confirm the diagnosis of eczema, your child’s doctor will ask questions concerning the rash and do a physical examination. Usually, no laboratory or skin tests are required to make the diagnosis.
Common Misunderstandings About Eczema
-
Eczema is not contagious or infectious, although it may be infected by bacteria due to constant scratching resulting in open sores.
-
Eczema not related to poor hygiene and is not a sign of poor parenting. In fact, overzealous washing with harsh antiseptics or soaps can be very drying and makes the condition worse.
-
Atopic eczema is not due to ‘bad blood’ or a result of what mothers have or have not done during pregnancy, neither is it due to lack of certain vitamins.
What to Avoid When Your Child has Eczema
- Excessive heat and perspiration
- Poorly moisturised skin. Avoid long periods in air-conditioned areas and frequent showers with hot water, which can worsen dry skin.
- Strong soaps, detergents, bubble baths
- Scratching (itch-scratch cycle)
- Excessive psychological stress which can lead to increased itch
- Allergies (e.g. food allergy esp in young children, house dust mite allergy)
- Skin colonization (occupying the skin surface and not causing infection) by the bacteria, Staphylococcus auerus (releases chemicals which worsens atopic eczema)
- Skin infection by bacterial (e.g. Staphylococcus aureus) or virus (e.g. herpes simplex virus)
- Woolen/nylon fabrics
- Insect/mosquito bites (the surrounding skin reaction can be worse than normal)
How Do I Treat My Child’s Eczema?
Some general advice for treating eczema include:- Very importantly, moisturise at least 3-4 times a day (more often if possible) with a fragrance-free moisturiser. Apply the moisturiser liberally over all skin surfaces, even on normal-looking skin. Your doctor will be able to recommend which moisturiser is suitable for your child.
- Avoid soap-based products.
- A moisturizing non-soap based body wash is recommended for patients with atopic eczema. Your doctor would be able to recommend which body wash is suitable for your child.
- Avoid long showers with hot water – limit shower time to 10 mins and use luke warm water instead.
- Consider an antiseptic wash to help reduce the skin colonization by the bacteria, Staphylococcus aureus. Family members may also require concurrent treatment with the antiseptic wash to reduce the chance of re-colonisation in the child.
- Reduce excessive perspiration, take showers after perspiring.
- Avoid scratching if possible, keep nails short and clean.
- Avoid woolen/nylon fabrics, wear cotton fabrics instead.
- Reduce the level of house dust mites. Wash bedsheets, pillow cases, and curtains in hot water (60 deg C) every 2 weeks. Avoid stuffed toys, thick curtains and carpets in the home.
Depending on the age of your child and the severity of eczema, specific treatments such as topical steroids, oral anti-histamines and oral/topical antibiotics are commonly prescribed as part of treatment.
Diaper Rash (Diaper Dermatitis or Nappy Rash)
Diaper rash refers to red and scaling skin rashes around the areas which are covered by the baby’s diapers. It is commonly seen in babies between 9 – 12 months of age, but may begin as early as 2 months.Does My Child Have Diaper Rash?
Diaper rash is commonly caused by Irritant Contact Diaper Dermatitis, from urine and faeces trapped in the diaper. It can also be caused by a yeast infection (Candida Diaper Dermatitis) or Seborrhoeic Diaper Dermatitis. Other less common causes include Impetigo, Perianal Streptococcal Disease and Allergic Dermatitis (caused by soaps, detergents or the diaper itself)

Depending on the cause of dermatitis, the appearance of diaper rash can vary. A rash caused by contact dermatitis is red and mostly appears on the backside but not the folds. However, a rash due to a yeast infection usually starts from the folds before spreading outwards. The rash is commonly associated with satellite lesions.
Symptoms of diaper dermatitis may be similar to other more serious conditions. Thus, it is advisable to consult your child’s paediatrician to get a proper assessment.
How Do I Treat My Child’s Diaper Rash?
Treatment may include:-
Frequent diaper change or removal of the diaper for a few days
-
Antifungal or antibiotic creams (as prescribed by your child’s doctor)
-
Anti-inflammatory creams (as prescribed by your child’s doctor)
-
Moisture-resistant diaper barrier creams (e.g. zinc oxide)
Proper skin care is very important in preventing diaper dermatitis. This includes:
Keeping the diaper area clean and dry
Changing diapers frequently
Allowing the diaper area to air dry at times
Limiting the use of soap and other harsh cleaners in the diaper area
3) Hives (Urticaria)

Hives (urticaria) is a condition in which red, itchy, and swollen areas appear on the skin, varying in size from small to large patches.
What Causes Hives?
In 80% of acute hives in children, an ongoing viral infection (e.g. common cold or flu virus) is usually the most common cause. However, it can also be due to allergic reactions from eating certain foods like shellfish, eggs, nuts, cow’s milk, soy, wheat or from medications like non-steroidal anti-inflammatory drugs (NSAIDS) e.g. Ibuprofen.How Do I Treat My Child’s Hives?
Viral hives typically last for 1-2 weeks before gradually resolving. For hives that are a result of an allergy, strictly avoid the food/medication trigger, but this should be done after consulting your child’s doctor. Your child’s doctor would commonly prescribe antihistamines to decrease the symptoms of hives, of which some may cause drowsiness as a side effect.4) Contact Dermatitis
Contact dermatitis is a physiological reaction that occurs when the skin comes in contact with certain substances. Irritants to the skin cause 80% of these reactions (also known as irritant contact dermatitis), while the remaining 20% are caused by allergens, which trigger an allergic response (also known as allergic contact dermatitis).What Triggers Contact Dermatitis?
- Urine and faeces in diapers (see Diaper Rash)
- Saliva
- Soaps and baby lotions
- Detergents
- Certain foods
- Plants (commonly poison ivy, poison oak)
- Metals (common metals include nickel, chrome and mercury)
- Latex (including products such as rubber toys, balloons, rubber gloves or pacifiers)
- Certain medications
Does My Child Have Contact Dermatitis?


Irritant contact dermatitis caused by wet wipes and licking (left) and from a nickel watch (right)
Contact dermatitis is typically most severe at the site of contact with the irritant. Symptoms can vary slightly depending on the child, but redness and swelling on the skin, blistering, itchiness and temporary thickening of the skin are usually observed.
Symptoms of contact dermatitis may resemble other serious skin conditions. If you are unsure, consult your child’s doctor for a clinical diagnosis.
How Do I Treat My Child’s Contact Dermatitis?
When identified, strictly avoid contact with the irritants. Wash skin with soap and water thoroughly after exposure. If your child has blisters, a cold compress may help relieve the itch and inflammation. Seek medical attention if the reaction is severe.5) Heat Rash (Prickly Heat or Miliara Rubra)
Heat rash or “prickly heat” occurs often during hot weather and humidity due to sweating and blockage of the sweat glands. It may also occur if the baby is overdressed or has a fever.
Heat rashes appear as little red bumps, similar to small blisters or pimples. The skin often feels prickly to the touch and commonly occurs in body creases or on areas where clothing rubs onto the skin, such as the neck, diaper area, armpits, upper back and chest.
How Do I Treat My Child’s Heat Rash?
Heat rash is harmless and should resolve in a couple of days once the child is cooled down. Remove excess clothing and bring your child to an air-conditioned room. A cool compress may help too. There is no need to put any topical medications because these may actually make the rash worse by causing the sweat glands be become more blocked.SUMMARY
Common Skin Conditions in Babies and Children include:- Eczema (Atopic Dermatitis)
- Diaper Rash (Diaper Dermatitis or Nappy Rash)
- Hives (Urticaria)
- Contact Dermatitis
- Heat Rash (Prickly Heat or Milaria Rubra)
About Author
This article is written by Dr Dave Ong, who completed his MBBS in the National University of Singapore (NUS) in 2009. He received his post-graduate specialist training in Paediatric Medicine at the National University Health System (NUHS) and was awarded the combined Master of Medicine (Paediatric Medicine) and Membership of Royal College of Paediatrics and Child Health (MRCPCH, United Kingdom) in 2014. Dr Ong is competent in paediatric and neonatal resuscitations for acute emergencies and has a special interest in respiratory, ear-nose-throat (ENT) and skin conditions.
Kids Clinic @ Punggol
681 Punggol Drive #03-11 Oasis Terraces Singapore 820681
Tel: (65) 6817 8885


